
Authors:

Dr. Nicole Culos-Reed, PhD, Associate Dean Graduate; EXCEL PI, Faculty of Kinesiology, University of Calgary 
Max Eisele, MSc, BSc in Exercise and Health Physiology
Cancer-related fatigue (CRF) is one of the most common side effects of cancer treatments. After curative cancer treatment, fatigue will improve and resolve over time for most people. However, for approximately 25% of individuals living with cancer, it may persist for months or years. We also know that for more advanced cancers, CRF tends to be more severe and negatively impacts quality of life.
How is CRF different from regular fatigue?
CRF is often described as a distressing, persistent sense of physical, emotional, and/or cognitive tiredness or exhaustion related to cancer or cancer treatment, that is not proportional to recent activity and interferes with usual functioning. This differs from commonly felt fatigue, which is usually proportional to recent activities and can easily be reversed by resting.
What causes CRF?
Unfortunately, there isn’t just one cause for CRF. Rather, based on current research we know that there are multiple contributing factors that may contribute to CRF. These include sleep disturbance, depression and anxiety, cancer therapies and medications, and many other potential physical and psychosocial factors.
What difficulties arise with CRF?
CRF can be difficult to talk about with family members, friends, and even your health care providers, as it is different from general fatigue and therefore often hard for others to fully understand. This may lead to frustration and isolation. It is important to learn how to share your difficulties coping with CRF with friends, family, or your healthcare provider, such as a rehabilitation oncologist. Sharing your CRF experiences will allow you to gather the support you need, and can help with others understanding your potential experiences and limitations in your daily activities.
What can help you cope with CRF?
There is strong and consistent evidence in the exercise oncology literature that physical activity and exercise help reduce CRF. However, engaging in any form of movement must follow the advice of “start low and progress slow”. Specifically, it is important that physical activity is built up over time, starting gradually (start low, with less than you think you can do). And then as you build up the ability to ‘move more’, you can increase the amount and intensity in small increments (progress slow), all the while being mindful of one’s energy levels.
| Research Spotlight Oberoi et al., 2018 1 Physical activity reduces fatigue in patients with cancer and hematopoietic stem cell transplant recipients: a systematic review and meta-analysis of randomized trials. • A systematic review of 170 studies • Physical activity reduced the severity of CRF • Different types of physical activity can be helpful in coping with CRF (e.g.: walking, fitness classes, strength training, yoga, and others) • Key is to find the activity you enjoy, can build into your usual routine, and that provides you with increased energy. • There is no ‘one size fits all’ approach – your exercise prescription must be tailored to you in order to optimize your benefits. |
What strategies can I use to stay active while coping with CRF?
To maintain being active and complete meaningful tasks in your everyday life, the three Ps might help:
Planning a day, or a week ahead of time, comes with many advantages. It allows you to schedule your most important activities, following them up with periods of rest to maintain an energy balance. Planning can also incorporate asking for help and ensuring you have the support you need.
Prioritizing is related to planning, with a focus on scheduling your activities based on how important they are to you. A good tip is to schedule your favourite activities during the time of the day when you have the most energy. Then you can feel good about getting in what is most important to you!
Finally, Pacing focuses on the balance between fatigue and energy levels. It is critical to listen to your body, and plan for periods of rest after expending energy. The main goal is to avoid “energy crashes”, by maintaining the balance between your energy and fatigue levels. A helpful tool you can use are these energy and fatigue thermometers:
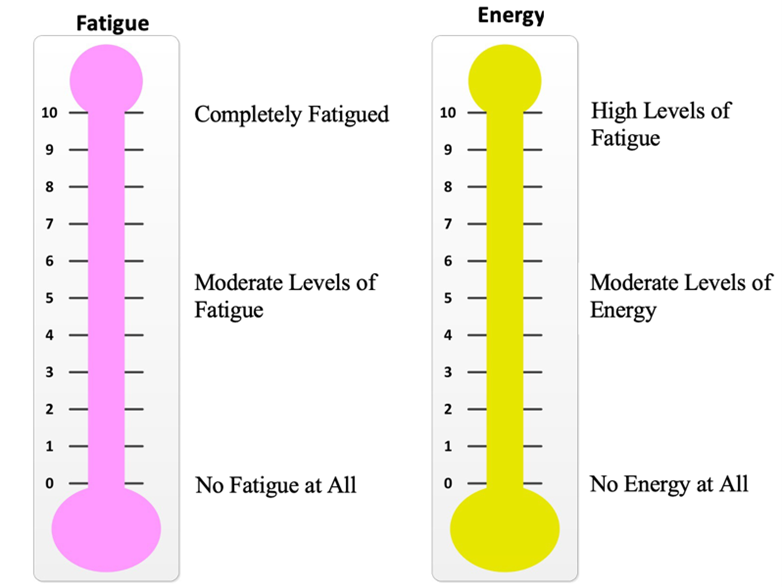
The fatigue/energy thermometers can be used throughout your day, or specifically pre, during, and post physical activity or your structured exercise sessions. Based on how you feel, adjust the intensity, duration, and type of activity.
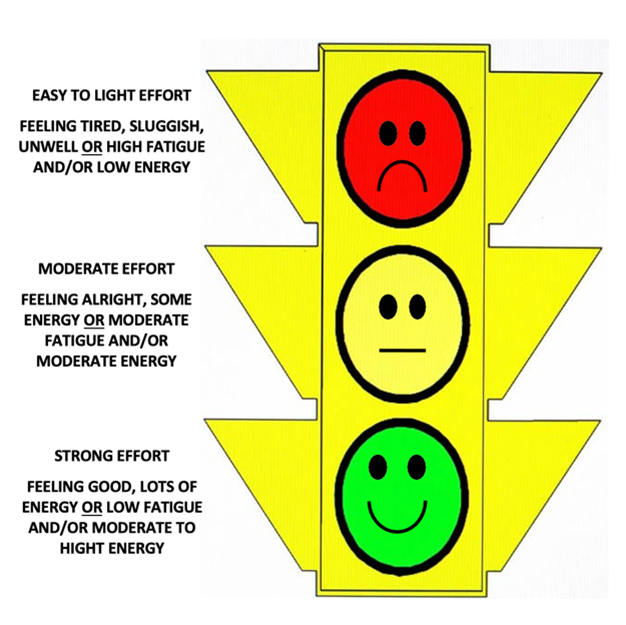
The Health and Wellness Lab uses our “Traffic Light System.” Green days are when you feel full of energy and have the energy to put into your exercise. These circuits are generally longer in duration and higher in intensity. Yellow days are on a day of moderate energy levels, whereas red days are on days of high fatigue and low energy. On a red day, doing any movement (such as household chores) or light activity (such as gentle yoga) may be all you need.
How much physical activity is enough?
Based on the current literature, we know at least a moderate intensity (moving enough to breath harder, break a sweat, or at a 4-6 on the RPE Scale) of physical activity helps individuals living with cancer manage their CRF2. Exercise sessions that are longer than 30 minutes have been shown to reduce CRF3. Finally, the recommended frequency of such exercise sessions is 2 to 3 times per week2, however, less than this recommendation may also already offer benefits1. These are general exercise prescription guidelines – work with a fitness professional to determine your tailored prescription, and what modifications you can make on your “red, yellow, or green light” days!
What specific activities other than exercise may be helpful?
The evidence shows that other tools, such as meditation, yoga and Tai Chi (which are forms of physical activity!) may also help you to manage your CRF. Other tools, such as sharing your thoughts and worries in prayer, support groups, or through journaling, may be beneficial. The key is to find what works for you – most individuals will try multiple resources to help them most effectively manage their CRF.
| Take-Home Messages • CRF is different from general fatigue. • Share your struggle with CRF and let friends and your healthcare team know what helps you manage it. • Use the 3 Ps (Planning, Prioritizing, and Pacing) to help you accomplish the daily tasks that are meaningful to you. • Exercise is an evidence-based tool that is one of your best options to manage your CRF. • Balance being physically active with periods of rest can help you manage your CRF. • Reach out to an exercise specialist for additional guidance. Contact us at wellnesslab@ucalgary.ca for more information. |
About the Authors:
Dr. Nicole Culos-Reed, PhD, Associate Dean Graduate; EXCEL PI, Faculty of Kinesiology, U of C
Dr. Nicole Culos-Reed, PhD, is a Professor, Director of the Health and Wellness Lab and the Thrive Centre. She is passionate about building movement into standard cancer care for all those living with cancer. You can find her on Twitter @NCulosReed or Instagram @activecdnmom.
Max Eisele, MSc, BSc in Exercise and Health Physiology
Max is a research assistant in the Health and Wellness lab whose research focus is on the benefits of physical activity maintenance and supporting cancer survivors to become physically active. During his Master of Science degree, Max has given several presentations on managing cancer-related fatigue to ACE and EXCEL participants.
References:
1) Oberoi S, Robinson PD, Cataudella D, et al. Physical activity reduces fatigue in patients with cancer and hematopoietic stem cell transplant recipients: A systematic review and meta-analysis of randomized trials. Crit Rev Oncol Hematol. Feb 2018;122:52-59. doi:10.1016/j.critrevonc.2017.12.011
2) Campbell KL, Winters-Stone KM, Wiskemann J, et al. Exercise Guidelines for Cancer Survivors: Consensus Statement from International Multidisciplinary Roundtable. Med Sci Sports Exerc. Nov 2019;51(11):2375-2390. doi:10.1249/MSS.0000000000002116
3) Meneses-Echavez JF, Gonzalez-Jimenez E, Ramirez-Velez R. Supervised exercise reduces cancer-related fatigue: a systematic review. Journal of physiotherapy. 2015;61(1):3-9.




