Authors:

Dr. Carla Prado, Professor of Human Nutrition and Registered Dietitian, University of Alberta 
Katherine Ford, MSc, Registered Dietitian 
Alena Frankish, BSc, PgD, Dietitian 
Emilia Grindlay, BSc
As various types of cancer become increasingly common worldwide, public interest in finding the best and most effective treatments is also growing. Chemotherapy, radiation, surgery, and a few other standard procedures are already well-established; yet, as we know, these often come with many downsides. It is not surprising then that people continue to seek other, non-traditional ways to treat cancer, one of which is the use of the ketogenic diet.
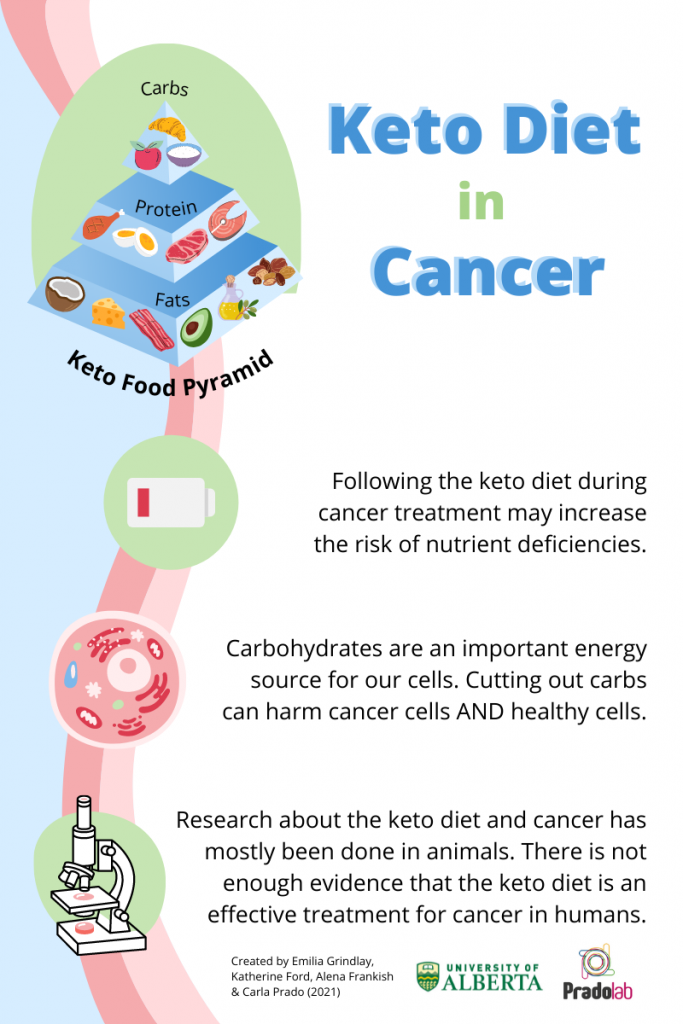
Why? The answer is rooted in carbohydrates. When we eat carbs, our body breaks them down into glucose. From what we know, cancer cells use a lot of glucose for fuel, and as such, some people think that by cutting carbohydrates out, we may be able to stop cancer from growing. Conveniently, the classic ketogenic diet is very low in carbohydrates (about 2% of the diet), while moderate-to-low in protein (8% of the diet) and high in fat (representing about 90% of the diet)1. Such a low amount of carbs cannot provide us with enough energy, thereby “forcing” the body to look for alternative sources. This in turn leads to ketosis, a unique metabolic state when we start burning fat for fuel and producing ketones. Since tumours cannot use ketones as a source of fuel, the ketogenic diet is thought to “starve the tumor”.
This pivotal question “Can you starve a cancer cell?” has sparked a lot of interest in the past few years, but the answer unfortunately is not that simple. On one hand, studies show that the ketogenic diet may help to slow tumor growth, ease inflammation, and help standard anti-cancer treatments work better2. On the other hand, most of the research on ketogenic diet in cancer was done in animals and the few studies that involved humans were small and provided conflicting results, making it difficult to draw concrete conclusions on its effectiveness in humans3. Furthermore, many animal studies suggest that not all tumours respond to the ketogenic environment in the same way and that some types of tumours will survive (or not respond at all) to this diet intervention4.
One of the biggest concerns with the ketogenic diet is that healthy cells also need glucose to survive, which means that cutting out carbs will impact both healthy cells and cancer cells. Therefore, if we simply eat too few carbohydrates, our body will still make glucose from other sources. Additionally, if protein intake is low (as in the ketogenic diet), our body will start breaking down its stores, which may further increase risk of muscle loss, a common complication associated with cancer.
Although more research is needed to weigh all risks and benefits of the ketogenic diet in cancer over the short and long terms, there are other dietary approaches that can strengthen the body and positively impact cancer treatment, quality of life, and survivorship5. For example, instead of cutting out carbs, choose healthier sources, such as whole grains, fruits and vegetables. These foods are rich in vitamins, minerals and antioxidants (substances that protect your cells by preventing or slowing damage). In contrast, carbohydrates from processed foods often have a lot of sugar and little nutritional value. You can also support your health by choosing protein-rich foods, such as lean meats, fish, eggs, cheese and legumes. These foods will help to build and maintain muscle mass and promote healing. Check out our post here about how to meet your protein needs and its importance. And of course, let’s not forget about the benefits of regular physical activity! Research shows that even small amounts of daily exercise can be helpful in maintaining strength and promoting appetite, while at the same time preventing fatigue, nausea and stress.
All in all, although ketogenic diet is being explored as a nutritional therapy to support cancer treatment, we still need much more research to understand the underlying mechanisms and to know when and how it can be used safely. Currently, ketogenic diet is not recommended by international, expert-based nutrition guidelines for people with cancer5. Eating a balanced diet that includes whole grains, fruits, vegetables and protein, while limiting processed foods with added sugar, salt, and saturated fats can be the best approach to support our immune system and promote overall quality of life.
Dr. Prado’s laboratory studies the importance of nutrition to cancer survivorship. They are particularly focused on developing targeted nutritional strategies to countermeasure low muscle mass in people with cancer. Follow Dr. Prado on Twitter, Instagram, and LinkedIn, and visit her website at www.drcarlaprado.com.
References
1) Allen BG, Bhatia SK, Anderson CM, Eichenberger-Gilmore JM, Sibenaller ZA, Mapuskar KA, Schoenfeld JD, Buatti JM, Spitz DR, Fath MA. Ketogenic diets as an adjuvant cancer therapy: History and potential mechanism. Redox Biol. 2014; 2:963-70. doi: 10.1016/j.redox.2014.08.002. Epub 2014 Aug 7. PMID: 25460731; PMCID: PMC4215472.
2) Weber DD, Aminzadeh-Gohari S, Tulipan J, Catalano L, Feichtinger RG, Kofler B. Ketogenic diet in the treatment of cancer – Where do we stand? Mol Metab. 2020 Mar; 33:102-121. doi: 10.1016/j.molmet.2019.06.026. Epub 2019 Jul 27. PMID: 31399389; PMCID: PMC7056920.
3) Oliveira CLP, Mattingly S, Schirrmacher R, Sawyer MB, Fine EJ, Prado CM. A Nutritional Perspective of Ketogenic Diet in Cancer: A Narrative Review. J Acad Nutr Diet. 2018 Apr;118(4):668-688. doi: 10.1016/j.jand.2017.02.003. Epub 2017 Mar 30. PMID: 28366810.
4) Goodwin J, Neugent ML, Lee SY, Choe JH, Choi H, Jenkins DMR, Ruthenborg RJ, Robinson MW, Jeong JY, Wake M, Abe H, Takeda N, Endo H, Inoue M, Xuan Z, Yoo H, Chen M, Ahn JM, Minna JD, Helke KL, Singh PK, Shackelford DB, Kim JW. The distinct metabolic phenotype of lung squamous cell carcinoma defines selective vulnerability to glycolytic inhibition. Nat Commun. 2017 May 26;8: 15503. doi: 10.1038/ncomms15503. PMID: 28548087; PMCID: PMC5458561.
5) Arends J, Bachmann P, Baracos V, Barthelemy N, Bertz H, Bozzetti F, et al. ESPEN guidelines on nutrition in cancer patients. Clin Nutr. 2017;36:11e48. doi: 10.1016/j.clnu.2016.07.015. PMID: 33487262